REFUNDS MANAGEMENT
Home / Refunds Management
Health Assistance is a guarantee in terms of efficiency and speed of service.

Health Assistance
Practices managed every year
0
+
In Health Assistance, the management of reimbursement procedures for its customers and clients is designed to allow for 4 different procedures, depending on the choices of the client and the chosen benefit.
If the coverage and procedural conditions are met, the Patient may request direct payment for the treatments that must be performed.
In order to request the activation of the procedure, at least 3 days before, the Patient must send the authorization request form accompanied by all the documentation relating to the treatments to be carried out for allow the medical staff and relevant offices to evaluate it.
Once the Patient has received the appropriate care (even if not through the structures affiliated with the Network), sends to Health Assistance the Reimbursement Request form and all the documentation relating to the treatments performed (invoices, notices , receipts, requests, requests, medical records, reports, etc…) to allow their evaluation by the medical staff and the relevant offices.
If the coverage and procedural requirements are met, but the chosen doctor does not appear to have an agreement with the Network, the Patient can request direct payment of the expenses relating to the Healthcare Facility and send, subsequently to reimbursement, the expense relating to the part of the medical team incurred for the same treatment event.
The Member who requires a service provided for by the Regulations signed in the Hospital Area section (hospitalization with or without surgery in an ordinary regime and daytime outpatient interventions, etc.), may submit a Request for Support from the Health Centre of Health Assistance by completing the form called “Nulla Osta Form: Request for Support for Hospital Services”.
Download the form here.
The health service at the Structure defined in the Nulla Osta can be booked by the Member following the release of authorization by the Health Centre, both for Direct assistance and for Indirect Assistance In Network. The member, therefore, will receive Authorization from the Centrale Salute to proceed with the Direct Assistance formula if the service falls within the guarantees of the Regulation.
The authorization constitutes a no impediment for the direct activation of the service.
Download the form here.
The health service at the Structure defined in the Nulla Osta can be booked by the Member following the release of authorization by the Health Centre, both for Direct assistance and for Indirect Assistance In Network. The member, therefore, will receive Authorization from the Centrale Salute to proceed with the Direct Assistance formula if the service falls within the guarantees of the Regulation.
The authorization constitutes a no impediment for the direct activation of the service.

The Health Center provides information and assistance regarding:
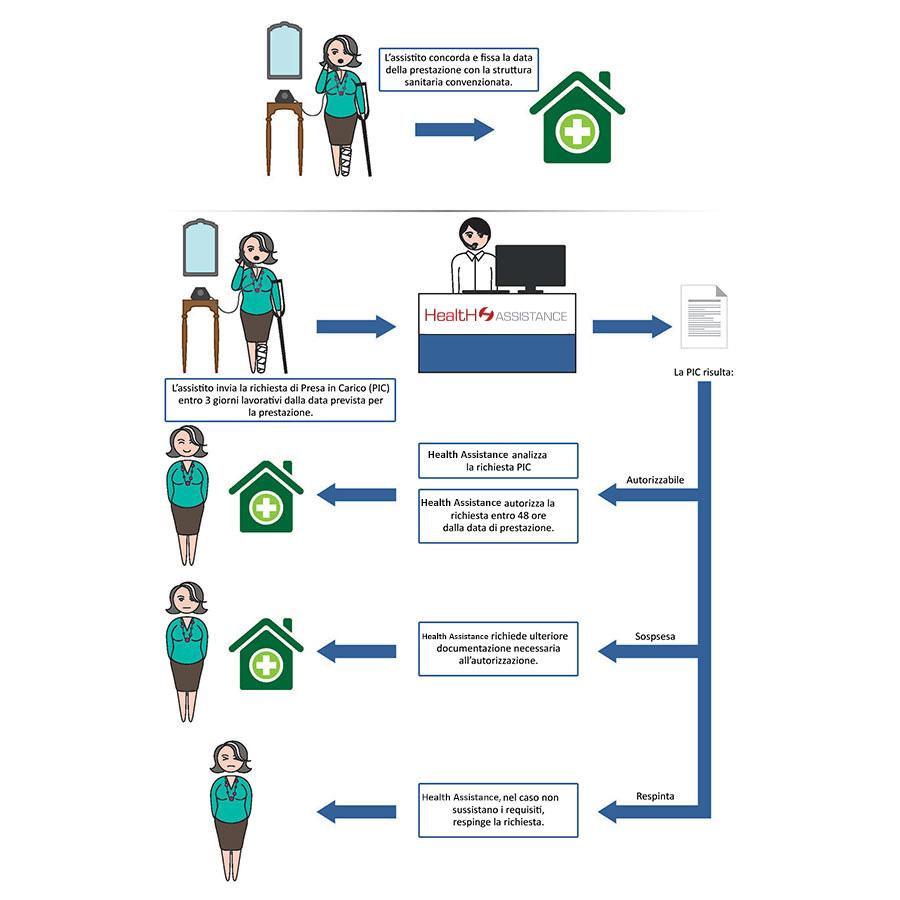
Direct Form - Authorisation Phase
In the case of the direct payment with taking charge (PIC), Health Assistance carries out the procedures only and exclusively with the pre-activation system: each Patient – after having directly booked the service – send the request for direct payment to the Health Centre, usually at least 3 days in advance, indicating the chosen healthcare facility and the doctor where possible.
Only after having positively evaluated the request, the Health Center will forward the authorization for direct payment to the Healthcare Facility, by sending the “TAKING IN CHARGE” document by email.
Only after having positively evaluated the request, the Health Center will forward the authorization for direct payment to the Healthcare Facility, by sending the “TAKING IN CHARGE” document by email.
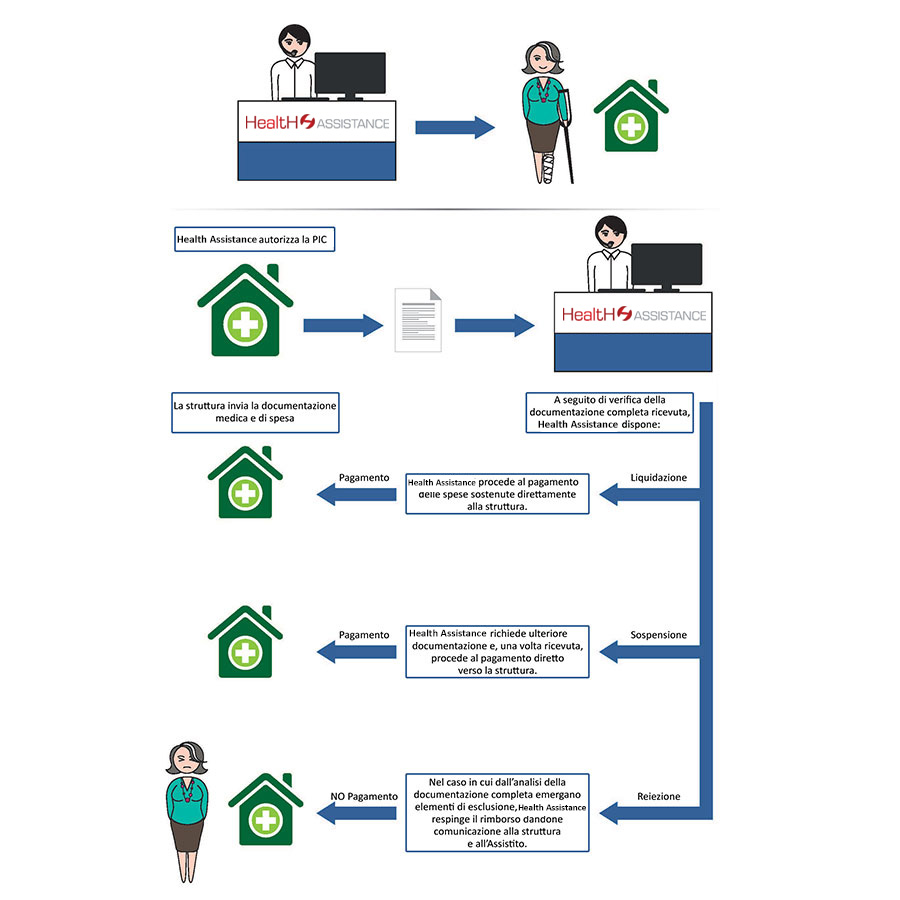
Direct Form - Liquidation Phase
Once the PIC has been authorized by Health Assistance and the service has been carried out, the Facility will forward to Health Assistance all the documentation relating to the treatments performed(invoices, notes, receipts, orders, requests, medical records, reports , etc…) to allow the medical staff and the relevant offices to verify.
If successful, the liquidation procedure for the Structure will be followed up.
If successful, the liquidation procedure for the Structure will be followed up.
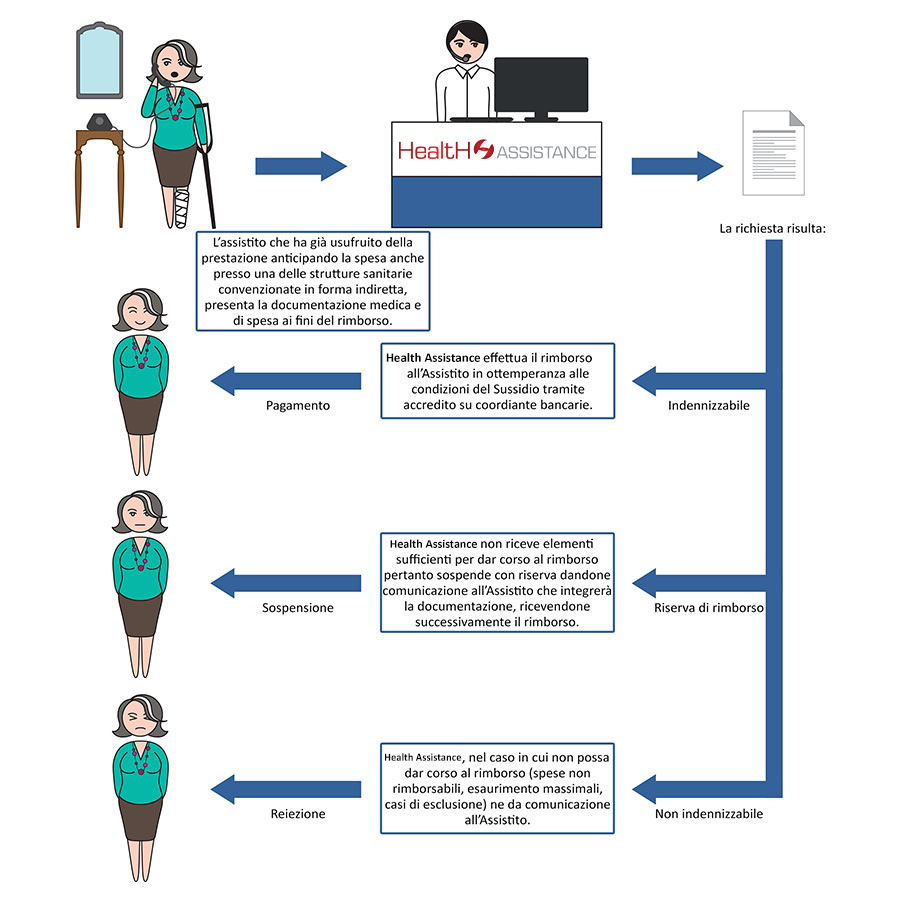
Indirect form
If the patient has already used the service by anticipating the expenses, present all the medical/health and tax documentation for reimbursement purposes.
If the procedure does not reveal an absence of documentation or elements that make the expense non-compensatable, the Health Assistance’s Settlement offices will proceed to initiate the reimbursement.
If the procedure does not reveal an absence of documentation or elements that make the expense non-compensatable, the Health Assistance’s Settlement offices will proceed to initiate the reimbursement.
Operating and ethical methods
TRANSPARENCY OF PROCEDURES
The system for managing and validating practices is the result of experience and allows adaptation to specific requests, "guiding" the operator in the procedures, optimizing operations and guaranteeing the timescales foreseen in the processing of the procedures.
Through the system it is possible:

Record the reasons for calling for an in-depth analysis of the needs of the population served.

Keep the "contact history" of the individual user under control, avoiding dispersion of information and speeding up the entire management of the procedures overall.

Transform inbound calls into outbound calls, thus allowing the Member/Patient to call back in the event of a queue, thus minimizing the waiting time and the non-response percentage.